The story of nurses and their COVID-19 experience
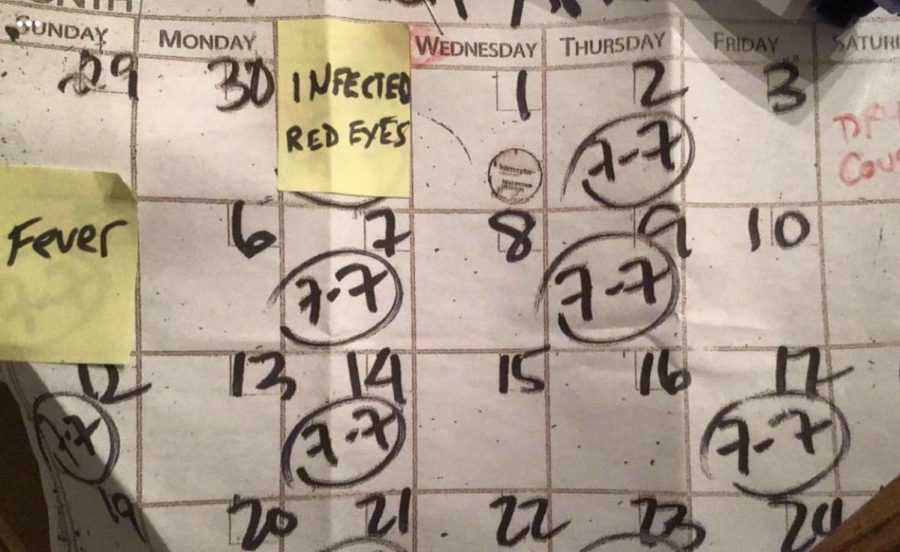
Zucker kept track of each of her symptoms during her quarantine process in April.
Amy Zucker is a Lane parent who works in the medical field and has been risking her life, working up to 4 days a week in the midst of the COVID-19 pandemic. Unfortunately, her work environment led to a positive COVID-19 test result after being switched to the COVID floor at her work.
Zucker is a registered nurse. She works in behavioral health and in-patient psychiatry. Working from 7 a.m. to 7:30 p.m. dealing with psychiatric patients, people who have thought disorders and people who struggle with addiction and homelessness.
When Zucker got COVID around April, her first symptom was conjunctivitis, inflammation of the membrane that covers the eyeball and inner eyelid. Then she realized she was coughing.
“I thought, you know, I’m coughing, I’m never sick. I better call in,” Zucker said. “And so I did what I normally wouldn’t and then the next day I had a temperature.”
“So I did one of those drive-through places that they still have,” Zucker said. “And I told them I’m a nurse. And so the turnaround was expedited, because they prioritized front line workers’ tests, but it still took maybe three or four days. And then I had it.
“I’d sit and stare out the window as I began to feel trapped,” Zucker continued, elaborating on her COVID experience. “And in one room, it was really hard to have nothing to do, but maybe watch TV. It was really depressing. So that’s why I think it’s affected so many of our patients.”
Zucker talked about the change in her work environment since COVID-19.
“Initially during March we were told we could not wear masks because we’re behavioral health nurses and our patients aren’t sick,” she said.
It wasn’t until one of her patients got COVID in April which resulted in nurses having to wear masks on the psych floor.
Zucker said her patients didn’t have to wear masks because of their strings that could be used for self harm.
Overall, Zucker said the safety procedures her work established are wearing face masks and social distancing, but it’s a struggle to do these things specifically where she works.
“I mean, in a lot of situations that we have, it’s really hard to follow those guidelines, with the social distancing and all that kind of stuff, that’s really hard to do,” Zucker said.
According to Zucker, the guidelines are hard to follow because of the kind of patients the hospital has — people who can become agitated, irritated, and violent. The nurses have to be right on top of them. There is no six feet when one has to hold somebody down and give them a shot or put them in restraints.
Zoe Zucker, Amy’s daughter, remembers when her AP World teacher told her she’ll have an exam the following Monday, when schools first closed in March due to the pandemic and nobody expected COVID to continue.
“I remember when I first heard of it, I was like, it’ll be fine. But that opinion quickly changed,” said Zoe, Div. 255.
Her reaction towards her mother’s positive test was posting it on Snapchat.
“I try to joke about stuff, but I don’t know,” she said. “I didn’t know if she’d be OK. But also, some people have had it really bad and almost died from it but she never really did.”
Shannon Dukes works at a rehabilitation center called Alden in Skokie, as an LPN, a licensed practical nurse. She is a nighttime nurse working from 7 or 11 p.m. to 7 a.m. addressing wounds, taking temperatures, checking medication, checking vitals and handling codes. She’s also studying at Ambria to become a registered nurse.
She got COVID in May.
“I got it at work, but it was weird because I was doing everything right,” Dukes said. “There was nothing we could have done wrong. I wore my mask, wore gloves, wore everything, but somehow along the way, I got it from there.”
Dukes said she is relatively certain that she contracted the virus from work; her family would rarely see her because of her nonstop schedule. She would come home when her family was asleep and rest while everyone was up. Her husband would do all the grocery shopping. Work was the only place she went.
Dukes faced a cold, her temperature would rise, she’d get bad headaches, and her taste and smell were completely gone.
Her experience through this tough time and what she goes through at work made her realize the younger generations aren’t taking the pandemic seriously. At first she was receiving older patients. Once she started going out, she saw younger people having parties, getting together, and hanging out with no masks. Younger patients starting coming in, getting their families sick.
“Everybody thought it was just older people getting it,” Dukes said. “And I’m only 33. So I was one of the youngest ones to get it at the time in my job. You guys don’t understand this is a serious thing.”
Leilani Dukes, Shannon’s daughter, was in Mexico in February when the first cases overseas were announced. She was scared because everyone was talking about it and she thought she wasn’t coming home, but she made it home safely.
Her mother then contracted COVID.
“She didn’t want us to worry about it, but I was definitely more worried about it because it’s something you don’t know about,” Leilani said. “Because at that point I would hear that nobody was surviving, this was around May, and now that you hear it people stay home and end up coming back. And so I thought, what am I going to do? If she does have it? It was a crazy thought.”
When her mom was ill, Leilani would put on her gloves and mask, then go into her mom’s room to give her a plate of food and other essentials.
“You shouldn’t take any person for granted,” said Leilani. “So I’m not saying go out there and go see that person but maybe call them and just be like, Hey, how’s it going? Because you’re never gonna know, you know, if they go out and they’re going to catch it.”
Your donations directly fund the Lane Tech student journalism program—covering essential costs like website hosting and technology not supported by our school or district. Your generosity empowers our student reporters to investigate, write, and publish impactful stories that matter to our school community.
This website is more than a publishing platform—it's an archive, a research tool, and a source of truth. Every dollar helps us preserve and grow this resource so future students can learn from and build on the work being done today.
Thank you for supporting the next generation of journalists at Lane Tech College Prep!